4. PSA
| Ward | Casualty Department | D.O.B/Age | 04/12/1940 |
| Consultant |
Prostate-specific Ag (PSA) 949.50 H ug/L <4.00
Urinary retention.
Request form: Lower urinary tract symptoms and urinary retention.
| Important clinical findings to assess for include: General: Temporal wasting, signs of urinary incontinence (e.g. any leaking noted, need to wear sanitary products) Abdominal: Assess for masses, palpable bladder from retention P.R: Assess prostate for size, consistency, tenderness. CNS: Assess for any neurological fallout as prostatic metastasis tend to metastasize to the lower vertebrae. |
Creatinine 83 umol/L 64 – 104
eGFR (MDRD formula) >60 mL/min/1.73 m2
White Cell Count 5.01 x 109/L 3.92 – 10.40
Red Cell Count 5.39 x 1012/L 4.50 – 5.50
Haemoglobin 15.5 g/dL 13.0 – 17.0
Haematocrit 0.485 L/L 0.400 – 0.500
MCV 90.0 fL 83.1 – 101.6
MCH 28.8 pg 27.8 – 34.8
MCHC 32.0 L g/dL 33.0 – 35.0
Red Cell Distribution Width 13.2 % 12.1 – 16.3
Platelet Count 226 x 109/L 171 – 388
PATHOLOGICAL DIAGNOSIS:
Prostate, biopsy: Adenocarcinoma.
Imaging studies may be necessary if there is a concern for metastasis and these will be guided by the clinical presentation e.g. CXR if metastasis to the lungs is suspected vs MRI if there is a concern of vertebral collapse.
Prostatic adenocarcinoma.
- Prostate-specific antigen (PSA) is a protein produced by normal prostatic cells. The majority of PSA is produced by the glands in the transitional zone of the prostate (BPH). The peripheral zone, where 80% of prostate cancers originate, produces very little PSA.
- An enlarged prostate can cause obstructive uropathy. The creatinine values in this patient do not suggest renal impairment though a baseline creatinine would be required to assess this.
- PSA is used for screening, diagnosis as well as monitoring of prostate related disease processes. PSA is an organ-specific, not a cancer-specific marker. It is useful in detection, staging and monitoring of prostate cancer.
- To improve diagnostic accuracy when PSA is between 4-10ug/L (“grey zone”), free PSA is measured and the free/total PSA ratio is calculated. Most normal PSA is protein-bound, and in prostatic cancer, a greater proportion is unbound. A free/total PSA ratio <0.25 increases the likelihood of cancer.
21. APT
| Ward | Maternity Ward | D.O.B/Age | 27 y.o |
| Consultant | Dr C. Hudson |
APT test positive.
?haemolytic disease of the newborn
27 y.o. female
G2P1 at 34 weeks
RH negative with Rhesus iso-immunization. Anti-D titres 1:128. (Blood group AB negative). Coombs test positive. Risk of haemolytic disease of the new-born.
Not applicable/difficult to examine foetus in-utero. Ultrasound of the middle cerebral artery peak systolic velocity was suggestive that the baby was anaemic.
U/s guided chordocentesis done and foetal blood sample obtained in utero. FBC whilst in utero showed Hb: 9.8.
Clinician requested APT test to ensure that foetal sample obtained during chordocentesis.
Haematology did Kleihauer Betke Test and it showed 100% foetal haemoglobin. APT test also correlated and showed foetal haemoglobin.
Ultrasound: middle cerebral artery peak systolic velocity suggestive that the baby was anaemic. U/s guided chordocentesis done and foetal blood sample obtained in utero. FBC whilst in utero showed Hb: 9.8.
APT test confirmed that foetal blood had been obtained during chordocentesis. It also correlated with the Kleihauer Betke done by haematology.
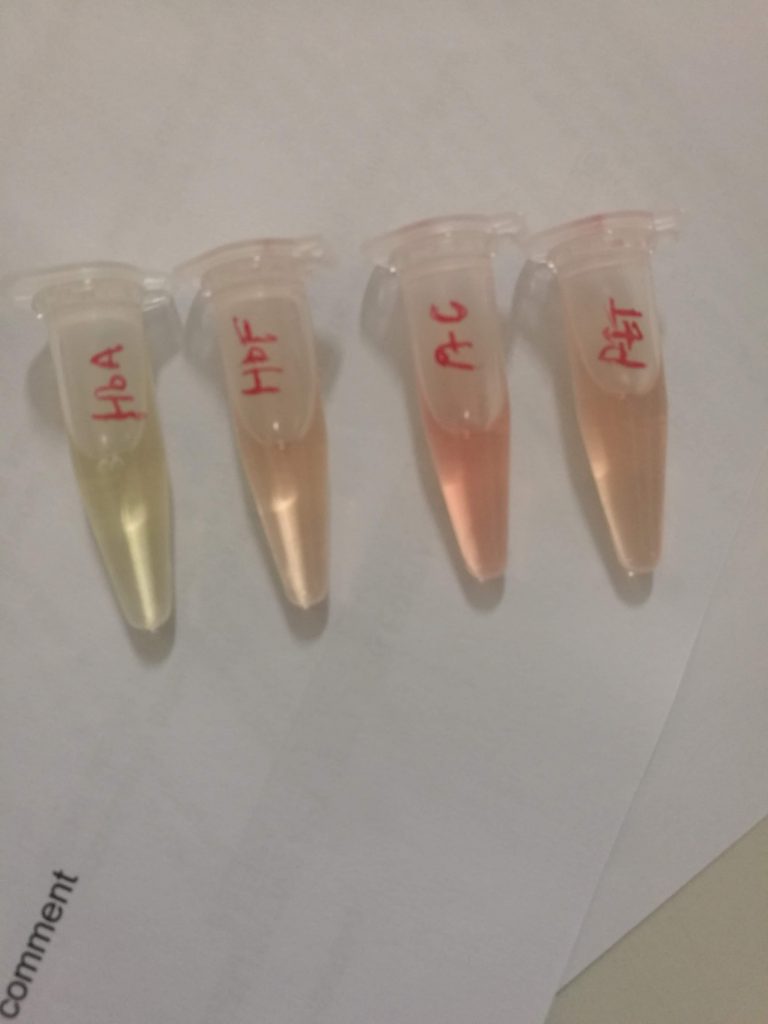
HbA: adult haemoglobin; HbF: foetal haemoglobin; PtC: patient control; PtT: test control.
Note the slight green tinge of HbA
Principles of the APT test: Sodium hydroxide (NaOH) denatures adult oxyhaemoglobin to haematin (with a colour change from pink to yellow green). Foetal haemoglobin resists alkaline denaturation by NaOH and maintains a pink colour. If adult haemoglobin (HbA) is present in the sample, it turns yellow and then green within two minutes of the addition of sodium hydroxide. Any pink colour that persists for longer than 2 minutes indicates foetal haemoglobin (HbF) is present in the sample.
The Kleihauer Betke Test is an acid-elution assay performed on maternal blood to determine the amount of HbF that has passed into maternal circulation. The process exposes maternal blood smear to an acid solution. HbF, being resistant to the acid, removes intact, whereas HbA is removed. Following this, the smear is stained via Shepard’s method. The foetal red blood cells are left rose-pink in colour, and the maternal cells appear “ghost-like” due to the absence of staining. This test is done by Haematology. Other ways of differentiating maternal from foetal blood is examining the MCV. The foetus has a larger MCV. This is nonspecific though as the mother may have macrocytic anaemia.
3. Hyperammonaemia
| Ward | Medical ward | D.O.B/Age | 16/07/1950 |
| Consultant |
Ammonia 251 H umol/L [11 – 35]
| Specimen request form has hepatic encephalopathy written as the diagnosis/reason for request. |
Unable to obtain.
Unable to obtain.
| Sodium 143 mmol/L [136 – 145] Potassium 4.4 mmol/L [3.5 – 5.1] Urea 28.1 H mmol/L [2.1 – 7.1] Creatinine 359 H umol/L [64 – 104] eGFR (MDRD formula) 15 mL/min/1.73 m2 INR 2.77 Total bilirubin 54 H umol/L [5 – 21] Conjugated bilirubin (DBil) 36 H umol/L [0 – 3] Alanine transaminase (ALT) 34 U/L [10 – 40] Aspartate transaminase (AST) 113 H U/L [15 – 40] Alkaline phosphatase (ALP) 105 U/L [53 – 128] Gamma-glutamyl transferase (GGT) 33 U/L <68 |
| Unremarkable CMP. Elevated WCC of 11 otherwise normal FBC. Further investigations not requested on Trakcare. ?patient discharge vs transfer vs demise |
| ?Fulminant liver cirrhosis |
?End stage liver disease
Most ammonia dealt with by the liver is produced by gut organisms. Protein degradation forms a smaller contribution. Ammonia in high concentrations is neurotoxic. It is detoxified by the liver to urea via means of the urea cycle, and urea is subsequently excreted in the urinePre-analytical factors including a delay in sample reception and sample not transported on ice may cause raised ammonia results.Other pre-analytical factors to consider include:
- No smoking by the person collecting the sample or the patient the sample is being collected from.
- Tourniquet should not be applied tightly or for too long (no tourniquet application ideal).
- Collected in an EDTA container.
- Must reach the lab within 15 to 20 minutes of being collected on ice.
- Patient should be fasted.
This patient has mildly deranged liver function tests and a prolonged INR suggesting liver disease which may be contributing to the hyperammonaemia. The unremarkable elevation in the liver enzymes may be due to a decrease of viable hepatocytes.
20. Alpha-foetoprotein
| Ward | Emergency unit | D.O.B/Age | 07/08/1968 |
| Consultant | Dr C. Hudson |
Request form: No clinical information provided
Unavailable.
Unavailable.
Sodium 130 L mmol/L 136 – 145
Potassium 3.7 mmol/L 3.5 – 5.1
Urea 2.9 mmol/L 2.1 – 7.1
Creatinine 64 umol/L 49 – 90
eGFR (MDRD formula) >60 mL/min/1.73 m2
Glycated haemoglobin (HbA1c):
Glycated haemoglobin (NGSP) 6.5 %
Glycated haemoglobin (IFCC) 48 mmol/mol
Estimated average glucose (eAG) 7.8 mmol/L
Calcium 2.20 mmol/L 2.15 – 2.50
Total protein 86 H g/L 60 – 78
Albumin 28 L g/L 35 – 52
Total bilirubin 26 H umol/L 5 – 21
Conjugated bilirubin (DBil) 25 H umol/L 0 – 3
Alanine transaminase (ALT) 65 H U/L 7 – 35
Aspartate transaminase (AST) 444 H U/L 13 – 35
Alkaline phosphatase (ALP) 568 H U/L 42 – 98
Gamma-glutamyl transferase (GGT) 662 H U/L <40 Lipase 91 H U/L 13 – 60
Alpha-feto protein (AFP) 545010.0 H ug/L 0.0 – 7.0
Thyroid stimulating hormone 6.61 H mIU/L 0.27 – 4.20
Thyroxine (free T4) 13.7 pmol/L 12.0 – 22.0
White Cell Count 8.93 x 109/L 3.90 – 12.60
Red Cell Count 2.92 L x 1012/L 3.80 – 4.80
Haemoglobin 9.4 L g/dL 12.0 – 15.0
Haematocrit 0.278 L L/L 0.360 – 0.460
MCV 95.2 fL 78.9 – 98.5
MCH 32.2 pg 26.1 – 33.5
MCHC 33.8 g/dL 32.7 – 34.9
Red Cell Distribution Width 19.5 H % 12.4 – 17.3
Platelet Count 246 x 109/L 186 – 454

Abdominal ultrasound +/- CT scan may be helpful in detecting presence of liver mass +/- intra-abdominal masses.
Final diagnosis
?Hepatocellular carcinoma
This case allowed me to become familiar with the concepts related to limitations of an assay. Having come across the need for dilution and the concept of high-dose hook effect, I found it interesting to see the gradual increase in AFP value as further dilutions were done. These are terms and concepts that this case allowed me to become familiar with.
Limit of Blank: This is the highest apparent analyte concentration expected to be found when replicates of a blank sample (containing no analyte) are tested. Detects “noise” that could interfere with the result.
Limit of Detection: This refers to the lowest analyte concentration likely to be reliably distinguished from the limit of blank and at which detection is feasible. LoD is determined using measured limit of blank, and test replicates known to contain a low concentration of an analyte.
Limit of Quantitation: This is the lowest concentration at which the analyte can not only be reliably detected but also at which some predefined goals for precision and bias are met. The LoQ may be equivalent to the LoD or it could be at a higher concentration. This is the limit that is clinically significant.
2. Creatine Kinase
| Ward | Pollsmoor Female Centre | D.O.B/Age | 10/10/1988 |
| Consultant |
Creatine kinase (CK) 265 070 H U/L 20 – 180
Request form: Unable to obtain on Equation document viewer. Differential diagnosis in this patient includes rhabdomyolysis, severe burns, myocardial injury or ischaemia.
History
Unavailable.
Unavailable.
Sodium 139 mmol/L 136 – 145
Potassium 3.8 mmol/L 3.5 – 5.1
Urea 2.6 mmol/L 2.1 – 7.1
Creatinine 63 umol/L 49 – 90
eGFR (MDRD formula) >60 mL/min/1.73 m2
Total protein 76 g/L 60 – 78
Albumin 46 g/L 35 – 52
Total bilirubin 6 umol/L 5 – 21
Conjugated bilirubin (DBil) 2 umol/L 0 – 3
Alanine transaminase (ALT) 317 H U/L 7 – 35
Aspartate transaminase (AST) 1727 H U/L 13 – 35
Alkaline phosphatase (ALP) 153 H U/L 42 – 98
Gamma-glutamyl transferase (GGT) 43 H U/L <40
Folder unavailable. No treating doctor listed.
Final diagnosis
Rhabdomyolisis (most likely secondary to blunt force trauma).
Creatine kinase is an enzyme primarily found in muscle tissue that catalyzes the conversion of creatine and adenosine triphosphate (ATP) into phosphocreatine and adenosine diphosphate (ADP). This reaction is reversible and thus phosphocreatine serves as a rapidly available source of ATP. When muscle tissue is stressed or inflamed, the sarcoplasmic membrane becomes permeable and leaks cytosolic enzymes like creatine kinase into the bloodstream. The differential diagnosis of an elevated CK concentration is long and complex. Musculoskeletal trauma, myocardial injury, infections, and drug-induced myositis are the most common causes encountered in general clinical practice. Aso worth noting in this patient is the AST is markedly elevated in comparison to the other liver enzymes. This, coupled with the elevated CK levels imply that quite significant muscle damage has occurred.
Making dilutions when results are appearing as having a greater than value on the analyzer is important. Creatine kinase is an enzyme that may be used to monitor the clinical condition of a patient. It may thus be useful to know exact values to be able to determine ongoing damage vs resolution. By preparing samples in dilution, this allows for a relatively accurate determination of the concentration of an analyte of interest by overcoming large reagent requirements.